Originally posted on the University of Cambridge’s Judge Business School website (2018).
3D printing holds great potential for hospitals, but a study co-authored at Cambridge Judge Business School cautions that such tech advances also risk tensions through workplace “boundary” disputes.
Three-dimensional printing, in which computers are used to layer or otherwise bond materials to create objects, has huge potential in fields ranging from healthcare to food to automobiles.
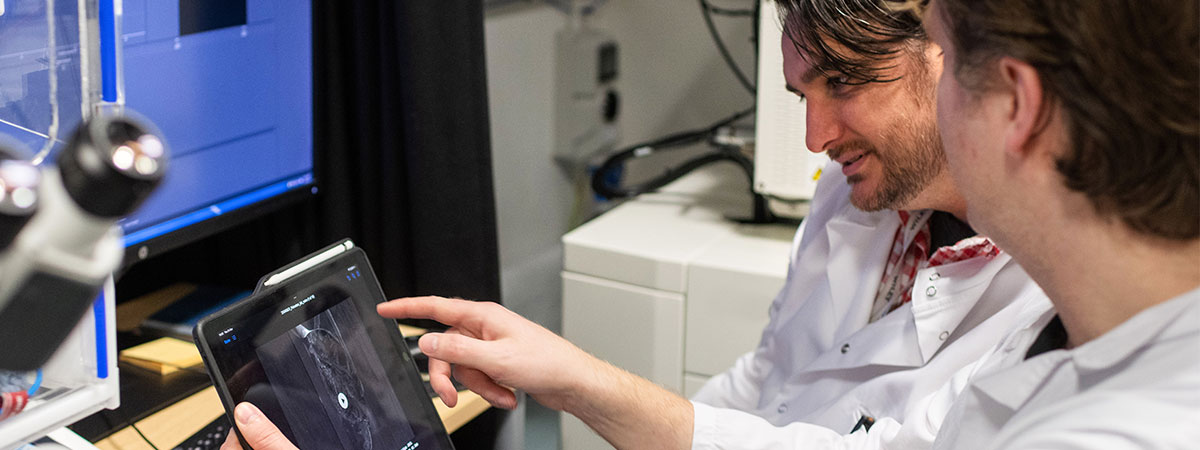
Hospitals have used 3D-printed anatomical models and implants to improve the predictability, safety, and speed of operations, in their quest for better quality and efficiency. Already, surgeons are using 3D printing to create patient-specific titanium plates that replace parts of patients’ skulls, rather than using traditional hand-hammered metal plates.
But what are the organisational ramifications of such a huge advance in technology, especially in the complex setting of a hospital where coordination among medical staff is so important to patient care and outcomes? How does this sort of innovation challenge professional boundaries, and what are the implications of such tensions?
New research by academics in the UK and Canada looks into this issue through a two-year study of how 3D printing was implemented at a British hospital organisation, including dozens of detailed interviews and hundreds of hours of observations. The study looks at four occupational groups: mechanical engineering technicians, radiologists and 3D printing technicians, clinical engineering R&D professionals, and neurosurgeons.
The working paper – entitled “A Pebble in Still Water: How Implementing 3D Printing Reconfigures Boundary Relations in a Hospital” – was presented at the annual conference of the Academy of Management in Chicago. A previous version of the paper won a “highly commended paper” award at the 11th Organizational Behaviour in Healthcare conference in Montreal.
The paper is co-authored by Michael Barrett, Professor of Information Systems & Innovation Studies at Cambridge Judge Business School, Stavros Polykarpou and Samer Faraj, Professor and Canada Research Chair in Technology, Management, and Healthcare at McGill University in Montreal.
Professor Michael Barrett of Cambridge Judge Business School discusses some of the paper’s findings:
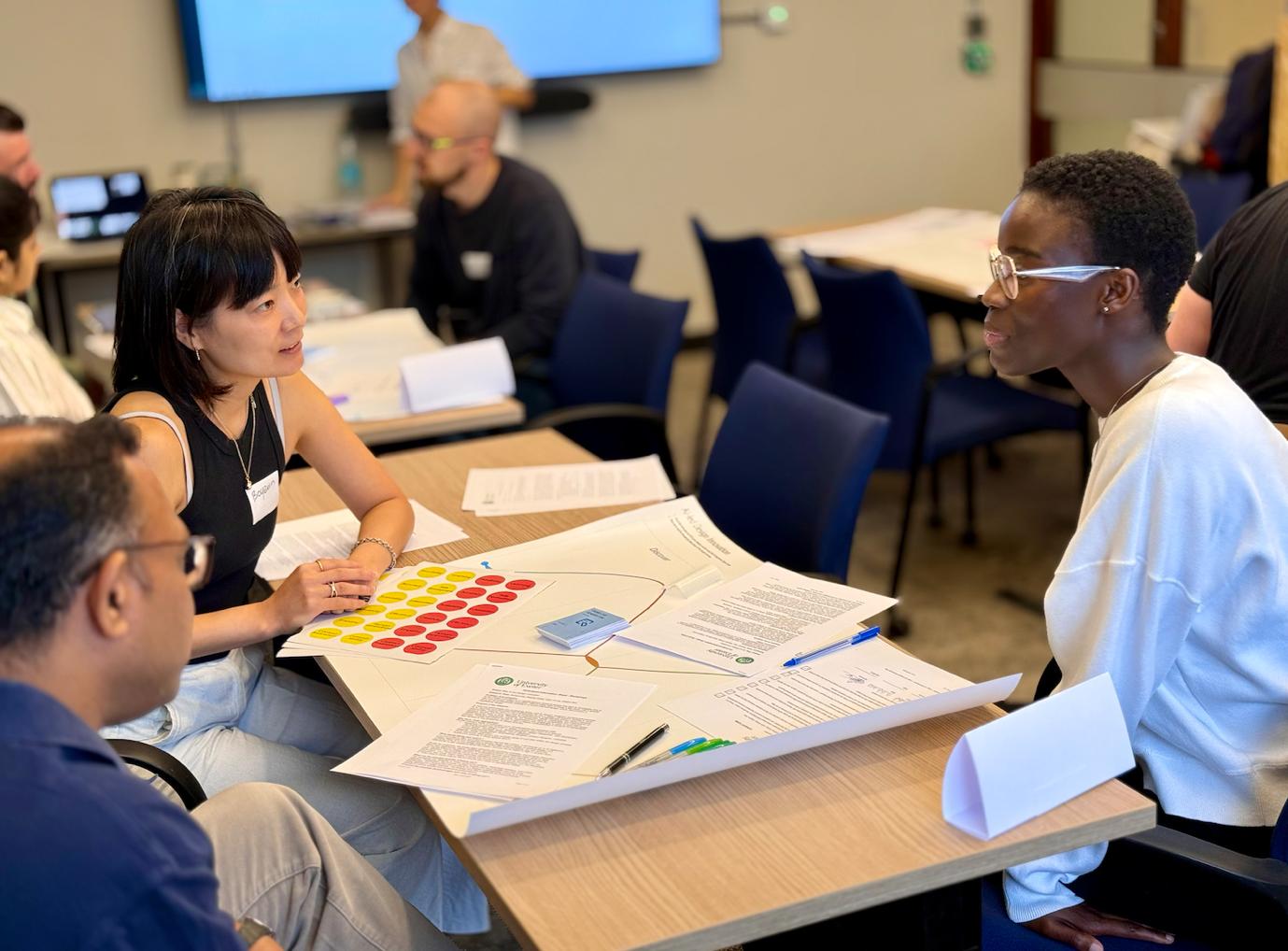
Healthcare is an ideal setting to study organisational “boundary” issues. The introduction of a new technology like 3D printing requires organising among a variety of occupational groups – including surgeons, radiologists, technicians, and R&D specialists. Hospitals have a high degree of stratification developed over many decades, and new procedures and technology can test that.
There was tension right away between the R&D Group and the mechanical engineering technicians. The introduction of 3D printing meant a reduction in more traditional engineering “manufacturing”, and an increase in the more scientific framework of R&D. A core activity of the R&D people was risk management, and this group sought to use its greater documentation skill to extend boundaries into areas previously occupied by the technicians and their two-dimensional drawings and machine tools – both in terms of new practices and also actual physical space. This resulted in frustration and a loss of status for the technicians.
Radiologists insisted that the 3D Laboratory be installed in a “neutral space” run by technicians rather than a specific department. This was designed to help ensure that 3D printing for anatomical modelling was available to the entire hospital, and not only to select surgeons or disciplines. The radiologists teamed with the 3D printing technicians to establish boundaries vis a vis the R&D Group.
The mechanical engineering technicians battled back. They argued that “traditional” machinery was still needed as much as ever to repair basic hospital equipment including beds and chairs, and sought a more balanced approach in introducing 3D technology.
Eventually, the 3D Laboratory ran into financial difficulty because it didn’t meet the numbers projected in its funding proposal. This initially led to greater collaboration between the various groups in a spirit of conciliation. Over time, the R&D Group again sought to stretch boundaries by drafting new accountability and quality control mechanisms for future 3D printing in hospitals.
For hospital managers, the findings underline the need to ensure collaboration in the face of new technologies. Cross-disciplinary collaboration among various medical professionals has always been at the heart of hospital care, and while technology can bring big advances it can also create unintended tensions that need to be effectively managed on an ongoing basis.